Body Dysmorphic Disorder DSM-5 Criteria
Get this Body Dysmorphic Disorder DSM-5 Criteria to diagnose BDD in patients, useful in mental health settings.


What is body dysmorphic disorder (BDD)?
Body dysmorphic disorder (BDD) is a mental disorder where a person becomes extremely worried about flaws in their appearance that might be minor or not even noticeable to others.
In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), BDD is classified under obsessive-compulsive and related disorders. It often coexists with eating disorders and frequently occurs alongside major depressive disorder, which can cause feelings of sadness and hopelessness. Other comorbidities include social anxiety disorder, obsessive-compulsive disorder, and substance-related disorder (American Psychiatric Association, 2013).
BDD symptoms include spending a lot of time checking their appearance or trying to hide perceived flaws, which can significantly impact their daily life and relationships. Body Dysmorphic Disorder (BDD) impacts roughly 1.7% to 2.9% of the general population, translating to between 5 million to almost 10 million individuals affected in the United States alone. Studies show it is more prevalent among women, comprising about 60% of those diagnosed, while men make up approximately 40% (Phillips, 2014).
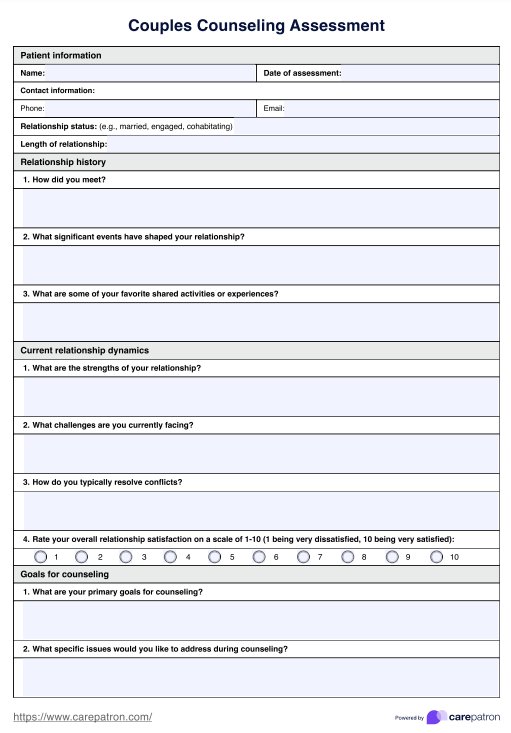
Body Dysmorphic Disorder DSM-5 Criteria Template
Body Dysmorphic Disorder DSM-5 Criteria Sample
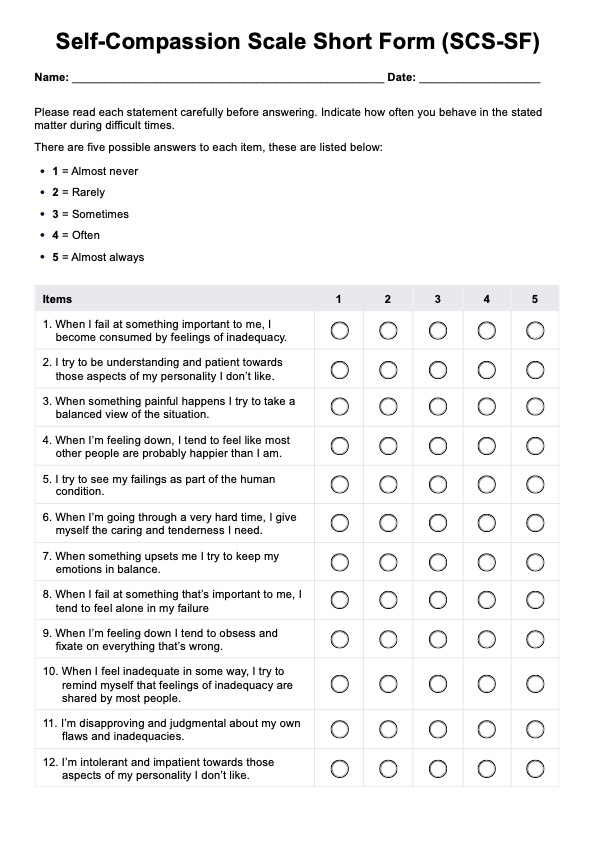
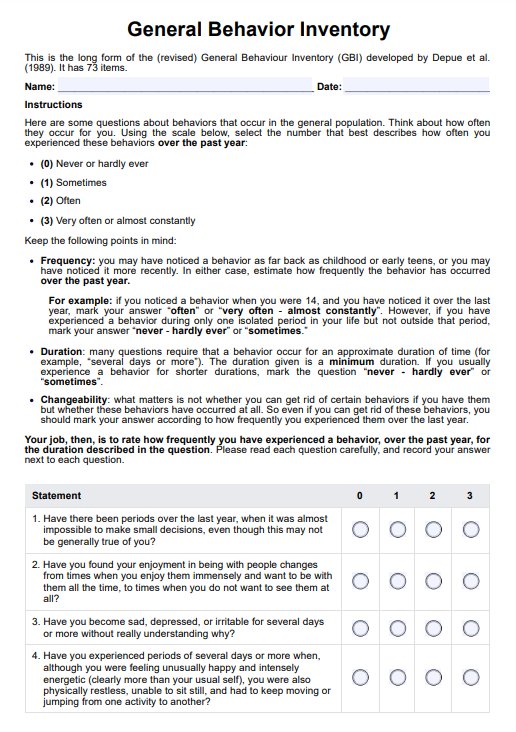
How is body dysmorphic disorder diagnosed?
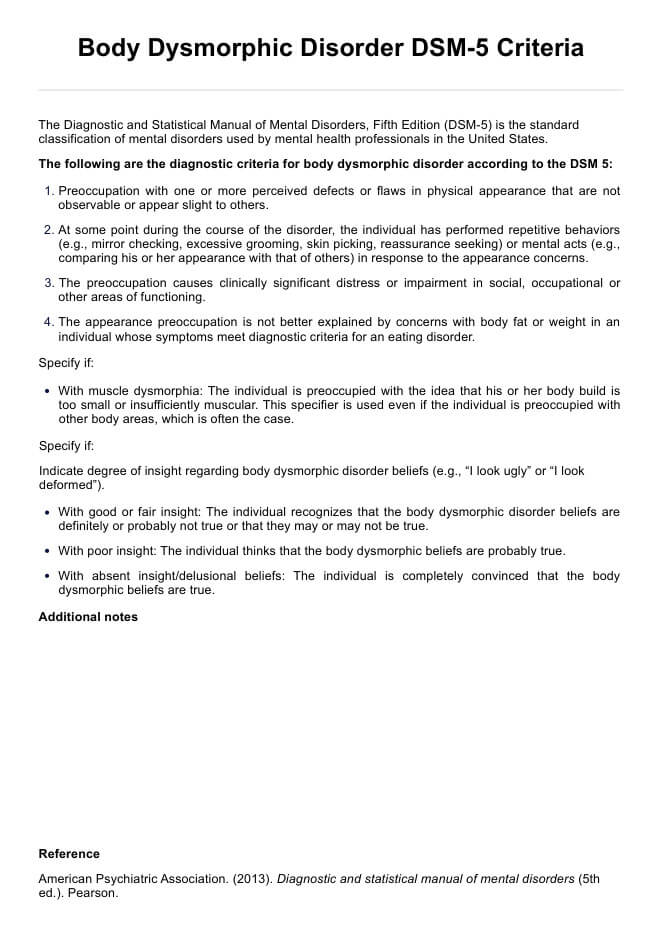
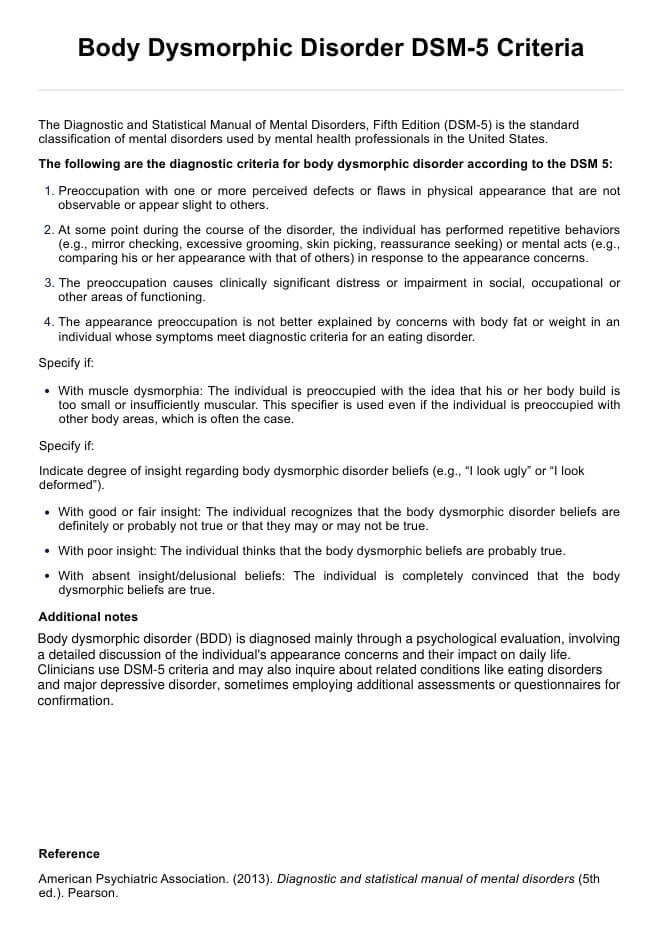
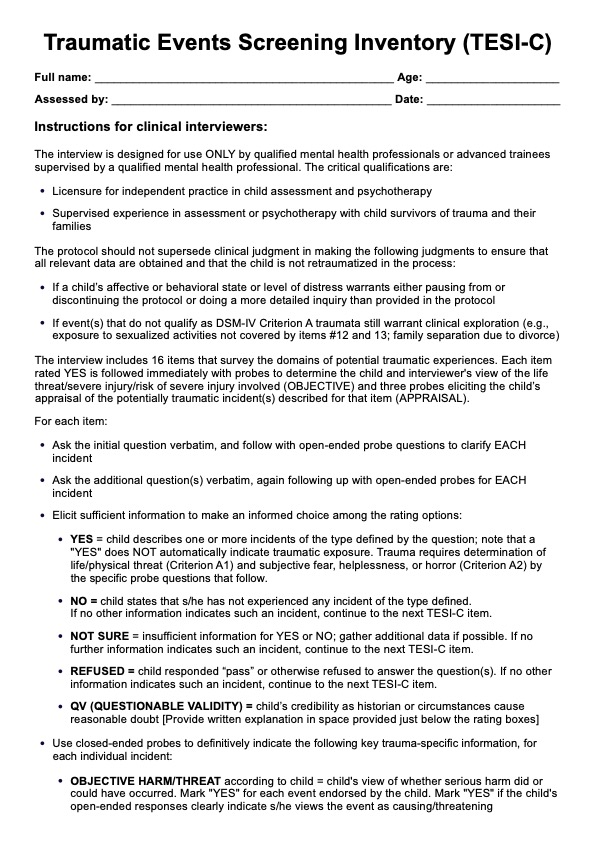
Body dysmorphic disorder (BDD) is diagnosed primarily through a psychological evaluation. The diagnosis involves a detailed discussion of the individual's concerns about their appearance and how these concerns affect their daily life and functioning.
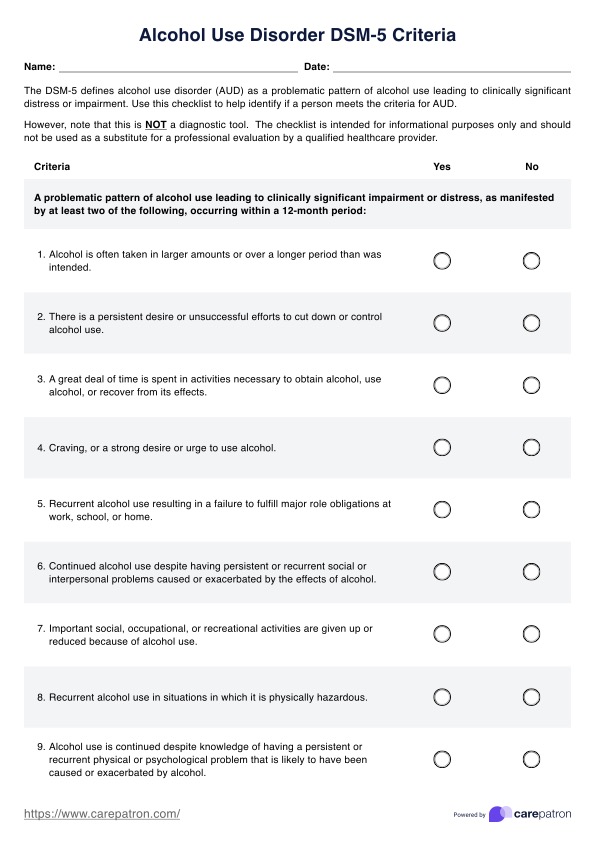
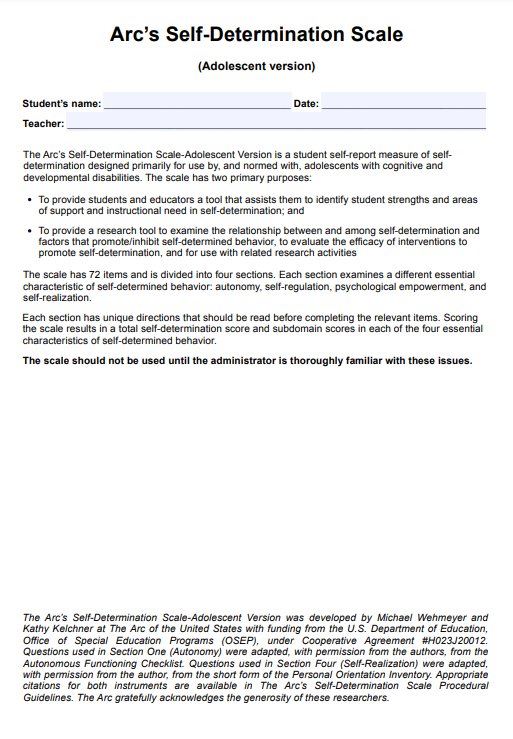
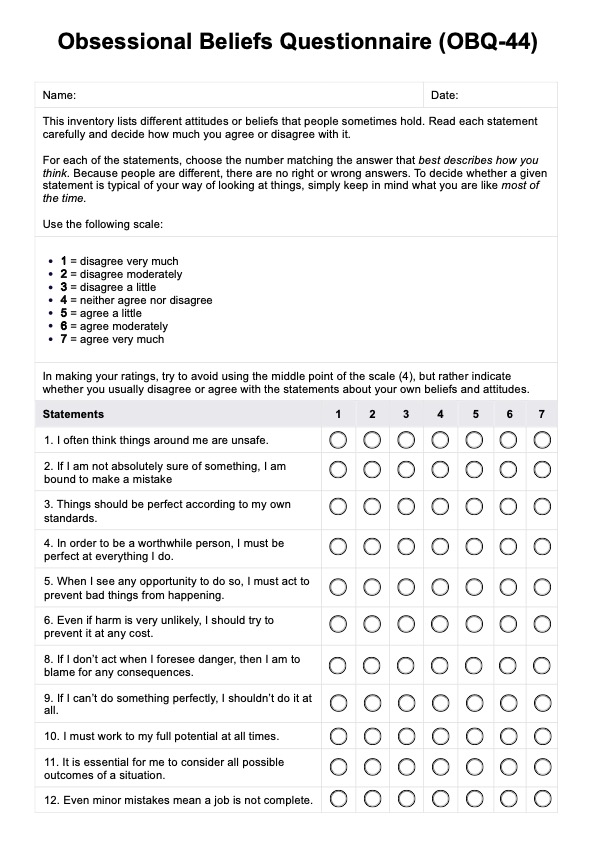
The clinician will typically use criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which outlines specific symptoms and behaviors characteristic of BDD. Inquiry about any related conditions, such as eating disorders or depression, that often coexist with BDD might also be performed. Sometimes, additional assessments or questionnaires may be used to gather more information and confirm the diagnosis.
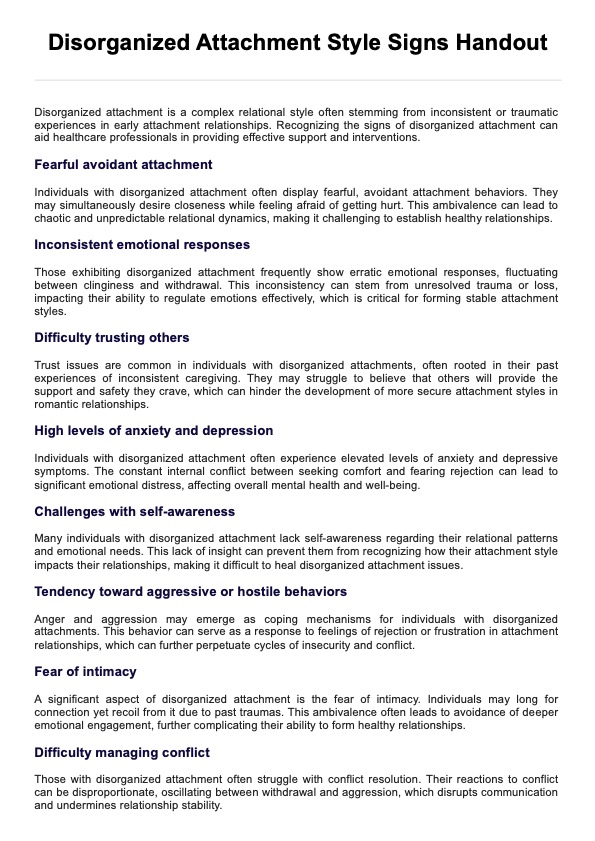
Body Dysmorphic Disorder DSM-5 diagnostic criteria
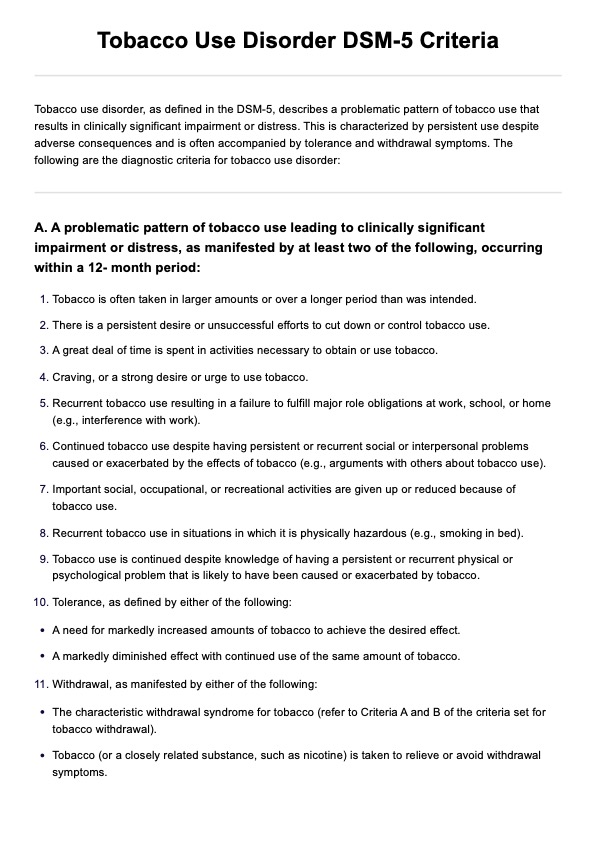
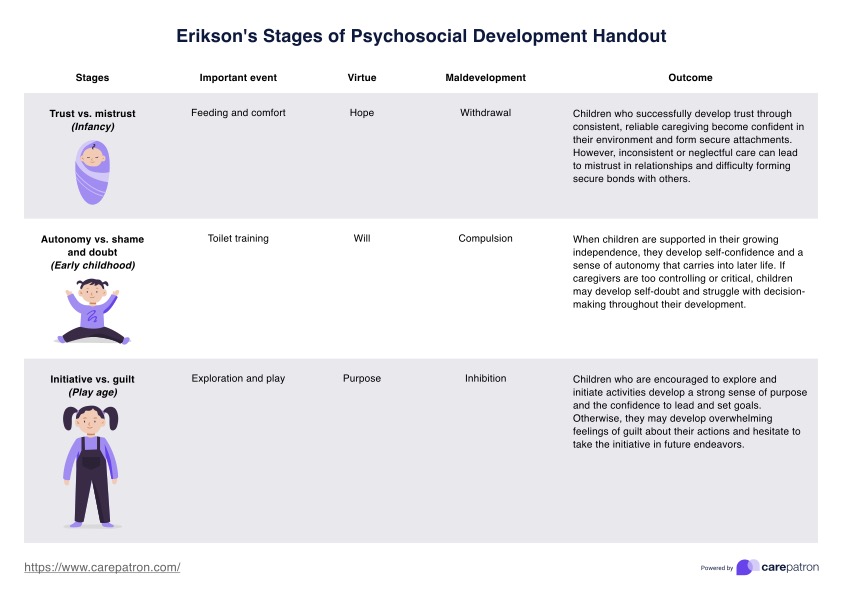
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is the standard classification of mental disorders used by mental health professionals in the United States (American Psychiatric Association, 2013a). The following are the diagnostic criteria for body dysmorphic disorder according to the DSM-5:
A. Preoccupation with one or more perceived defects or flaws in physical appearance that are not observable or appear slight to others.
B. At some point during the course of the disorder, the individual has performed repetitive behaviors (e.g., mirror checking, excessive grooming, skin picking, reassurance seeking) or mental acts (e.g., comparing his or her appearance with that of others) in response to the appearance concerns.
C. The preoccupation causes clinically significant distress or impairment in social, occupational, or other areas of functioning.
D. The appearance preoccupation is not better explained by concerns with body fat or weight in an individual whose symptoms meet diagnostic criteria for an eating disorder.
Specify if:
- With muscle dysmorphia: The individual is preoccupied with the idea that his or her body build is too small or insufficiently muscular. This specifier is used even if the individual is preoccupied with other body areas, which is often the case.
Specify if:
Indicate degree of insight regarding body dysmorphic disorder beliefs (e.g., "I look ugly" or "I look deformed").
- With good or fair insight: The individual recognizes that the body dysmorphic disorder beliefs are definitely or probably not true or that they may or may not be true.
- With poor insight: The individual thinks that the body dysmorphic beliefs are probably true.
- With absent insight/delusional beliefs: The individual is completely convinced that the body dysmorphic beliefs are true.
Differences between the DSM-4 and DSM-5 criteria
DSM-4 only outlines three criteria, and BDD is classified under somatoform disorders. In DSM-5, body dysmorphic disorder includes new criteria for repetitive behaviors (criteria B) in response to appearance concerns, reflecting their significance in diagnosis.
Unlike in DSM-4, the new edition introduces a specifier for "muscle dysmorphia" to acknowledge its clinical relevance. The delusional variant now falls under a specific specifier for absent insight/delusional beliefs, distinct from somatic delusions (American Psychiatric Association, 2013b; Substance Abuse and Mental Health Services Administration, 2016).
How is body dysmorphic disorder treated?
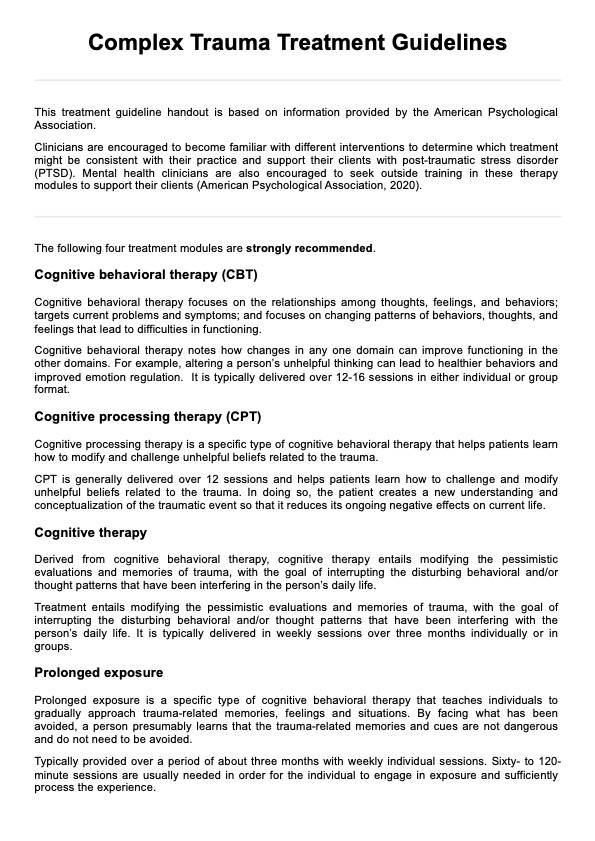
Body dysmorphic disorder (BDD) is typically treated using a combination of therapies aimed at reducing obsessive thoughts and improving overall well-being. Cognitive behavioral therapy (CBT) and the use of an antidepressant selective serotonin reuptake inhibitors are most common (Veale & Singh, 2019).
Cognitive behavioral therapy (CBT)
CBT supports patients by teaching them how to recognize and question negative thoughts about their appearance, replacing them with more realistic and positive beliefs. This therapy also involves methods to slowly lessen habits like repeatedly checking or fixing appearance issues and encouraging healthier ways to manage worries.
Selective serotonin reuptake inhibitors (SSRIs)
This is a type of medication that works by increasing serotonin levels in the brain, which can help alleviate symptoms of anxiety and depression often associated with BDD. They are prescribed to reduce the intensity of obsessive thoughts and compulsive behaviors related to appearance concerns.
References
American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (5th ed.). Pearson.
American Psychiatric Association. (2013b). Highlights of changes from DSM-IV-TR to DSM-5. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM_Changes_from_DSM-IV-TR_-to_DSM-5.pdf
Phillips, K. (2022). Prevalence of BDD. International OCD Foundation. https://bdd.iocdf.org/professionals/prevalence/
Substance Abuse and Mental Health Services Administration. (2016, June). Table 23, DSM-IV to DSM-5 body dysmorphic disorder comparison. https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t19/
Veale, D., & Singh, A. R. (2019). Understanding and treating body dysmorphic disorder. Indian Journal of Psychiatry, 61(7), 131–135. https://doi.org/10.4103/psychiatry.indianjpsychiatry_528_18
Commonly asked questions
Symptoms of body dysmorphic disorder include excessive worry about perceived flaws in appearance, frequent mirror checking, and avoiding social situations due to self-consciousness.
Body dysmorphic disorder is classified among the obsessive-compulsive and related disorders in the DSM-5.
Dysmorphia refers to a distorted view of one's body, while dysphoria is a general feeling of dissatisfaction or unease.





-template.jpg)