Oppositional Defiant Disorder DSM-5 Criteria
Access an Oppositional Defiant Disorder DSM-5 Criteria PDF as a reference tool in the clinical process.


What is oppositional defiant disorder?
Oppositional defiant disorder (ODD) is a behavioral disorder characterized by persistent patterns of anger, irritable mood, argumentative behavior, and vindictiveness towards authority figures. Children with ODD often display defiant, disobedient, and hostile behavior that significantly impairs their social, academic, and family functioning.
The disorder typically emerges in childhood or early adolescence and can persist into adulthood if left untreated. ODD is distinct from normal childhood defiance and requires a consistent pattern of behavior lasting at least six months for diagnosis (American Psychiatric Association, 2013a). Early identification and intervention are crucial for managing symptoms and improving long-term outcomes.
Oppositional Defiant Disorder DSM-5 Criteria Template
Oppositional Defiant Disorder DSM-5 Criteria Example
How is oppositional defiant disorder diagnosed?
Oppositional defiant disorder is diagnosed using the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The diagnosis requires a persistent pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness lasting at least six months.
These behaviors must occur with at least one individual who is not a sibling and cause significant impairment in social, educational, or occupational functioning. The frequency and intensity of symptoms should exceed what's typical for the individual's developmental level and cultural context.
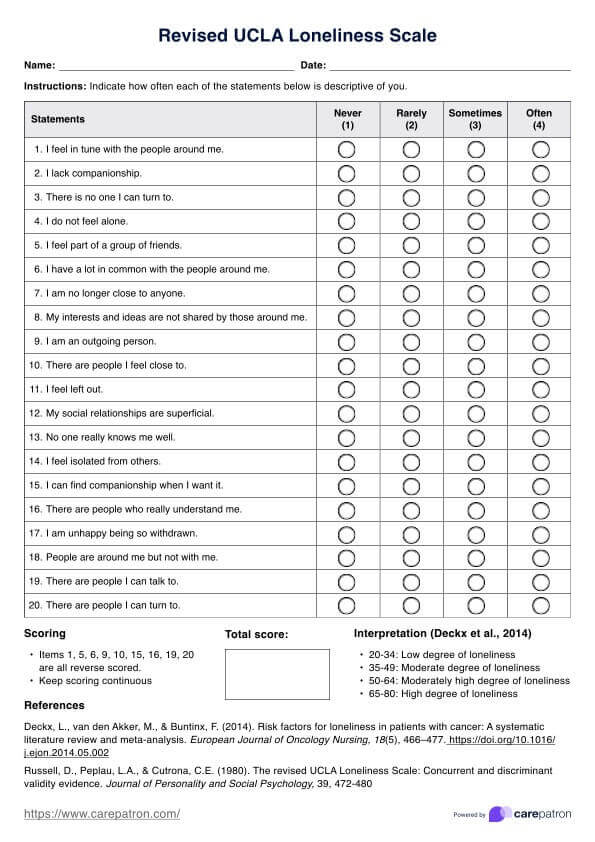
Clinicians must also rule out other potential causes of the behavior, such as substance use disorders or mood disorders. A comprehensive evaluation, including interviews with the child and caregivers, behavioral observations, and standardized rating scales, is essential for accurate diagnosis.
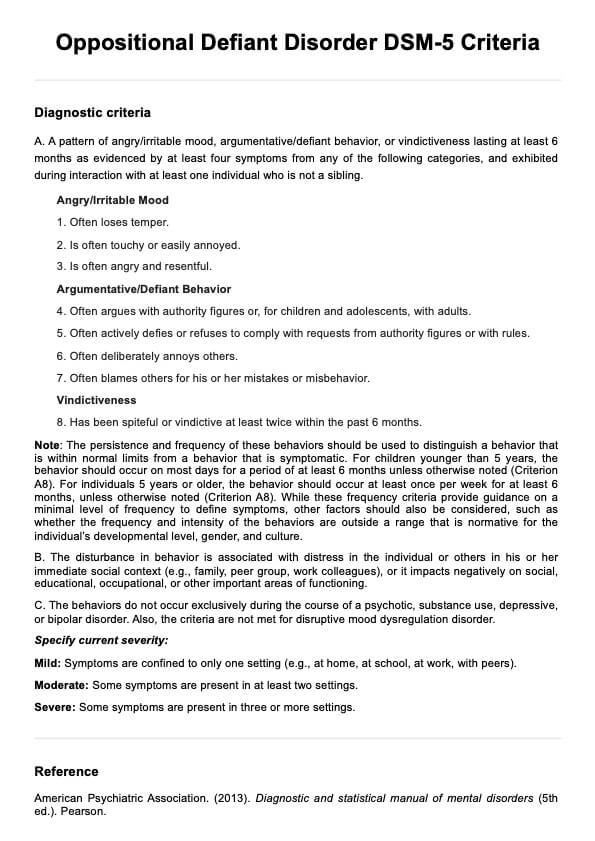
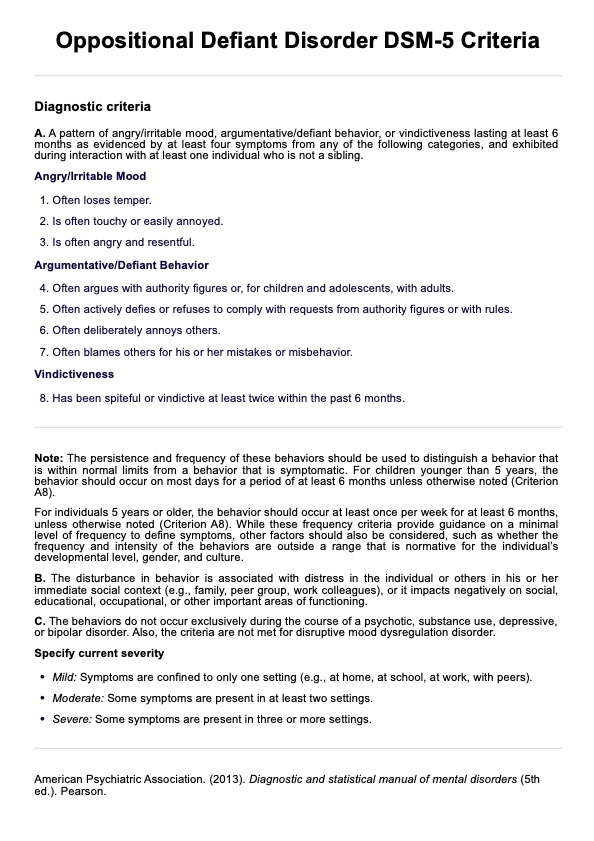
DSM-5 oppositional defiant disorder diagnostic criteria
The following criteria must be noted for an individual to be diagnosed with oppositional defiant disorder:
A. A pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness lasting at least 6 months as evidenced by at least four symptoms from any of the following categories, and exhibited during interaction with at least one individual who is not a sibling.
- Often loses temper.
- Is often touchy or easily annoyed.
- Is often angry and resentful.
- Often argues with authority figures or, for children and adolescents, with adults.
- Often actively defies or refuses to comply with requests from authority figures or with rules.
- Often deliberately annoys others.
- Often blames others for his or her mistakes or misbehavior.
- Has been spiteful or vindictive at least twice within the past 6 months.
B. The disturbance in behavior is associated with distress in the individual or others in his or her immediate social context (e.g., family, peer group, work colleagues), or it impacts negatively on social, educational, occupational, or other important areas of functioning.
C. The behaviors do not occur exclusively during the course of a psychotic, substance use, depressive, or bipolar disorder. Also, the criteria are not met for disruptive mood dysregulation disorder.
Differences between the DSM-4 and DSM-5 criteria
The DSM-5 has introduced four key updates to the diagnostic criteria for ODD (American Psychiatric Association, 2013b):
- Symptom categorization: The symptoms are now organized into three distinct groups: angry/irritable mood, argumentative/defiant behavior, and vindictiveness. This restructuring emphasizes that ODD encompasses both emotional and behavioral components.
- Conduct disorder coexistence: The previous exclusion of conduct disorder has been eliminated, recognizing that these conditions can co-occur.
- Frequency guidance: The criteria now include guidelines on the frequency required for a behavior to be considered clinically significant, acknowledging that some ODD-like behaviors are common in typical development.
- Severity rating: A new severity scale has been incorporated based on research indicating that the extent to which symptoms manifest across different settings is a crucial indicator of the disorder's intensity.
Differential diagnosis and comorbidities
ODD frequently co-occurs with other mental health conditions, which can complicate the diagnostic process and treatment planning. This is why understanding the relationship of oppositional behavior with other disorders is important for mental health professionals.
Attention-deficit/hyperactivity disorder (ADHD)
This is one of the most common comorbidities. The presence of ADHD can exacerbate oppositional behaviors and may require specific treatment considerations.
Mood disorders
Mood disorders, particularly depression and anxiety disorders, often co-occur with ODD. It's crucial to distinguish between irritability stemming from a mood disorder and the persistent angry/irritable mood characteristic of ODD. Disruptive Mood Dysregulation Disorder (DMDD) shares some features with ODD but is characterized by more severe and chronic irritability and temper outbursts.
Conduct disorder
Conduct disorder (CD) represents a more severe form of disruptive and aggressive behaviors and may develop from ODD in some cases. While ODD involves defiance and hostility, CD is marked by more serious violations of social norms and the rights of others, which can also develop into antisocial personality disorder later on.
Autism spectrum disorder
Autism spectrum disorder (ASD) can sometimes present with behaviors that mimic ODD symptoms. However, in ASD, these behaviors typically stem from difficulties with social communication and inflexibility rather than intentional defiance.
Language disorders or learning disabilities may also contribute to apparent oppositional behaviors. Children with these challenges may appear defiant when they struggle to understand or comply with instructions.
How is oppositional defiant disorder treated and managed?
Treating and managing ODD typically involves a comprehensive, multimodal approach tailored to the individual's needs and family circumstances. The most effective interventions often combine psychosocial treatments with family-based strategies.
Parent management training (PMT)
This is a cornerstone in ODD treatment. This approach teaches parents effective techniques to manage their child's behavior, reinforce positive actions, and improve parent-child interactions. Programs like the Incredible Years and parent-child interaction therapy have shown significant success in reducing oppositional behaviors.
Cognitive behavioral therapy (CBT)
CBT helps individuals develop problem-solving skills, emotion regulation, and social competence. It can be delivered individually or in group settings and focuses on anger management and interpersonal skills.
Family therapy
Family therapy can address broader family dynamics that may contribute to or maintain oppositional behaviors. Approaches like functional family therapy work to improve communication and problem-solving within the family unit.
It's important to note that treatment should be individualized, considering the child's age, symptom severity, and co-occurring conditions. Early intervention and consistent application of behavioral strategies across home and school environments are key to improving long-term outcomes for children with ODD.
References
American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (5th ed.). Pearson.
American Psychiatric Association. (2013b). Highlights of changes from DSM-IV-TR to DSM-5. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM_Changes_from_DSM-IV-TR_-to_DSM-5.pdf
Commonly asked questions
A child diagnosed with oppositional defiant disorder (ODD) is most likely to exhibit a pattern of angry or irritable mood, argumentative or defiant behavior, and vindictiveness towards authority figures. This may include frequent temper tantrums, refusal to comply with rules, blaming others for their mistakes, and deliberately annoying others.
To diagnose oppositional defiant disorder (ODD), a mental health professional typically conducts a comprehensive assessment that includes a clinical interview, behavioral observations, and standardized rating scales cross-referenced with diagnostic criteria in the DSM-5.
Oppositional defiant disorder (ODD) and attention-deficit/hyperactivity disorder (ADHD) are distinct but often co-occurring conditions. ODD is characterized by a pattern of defiant and oppositional behaviors, such as arguing with authority figures and being easily annoyed, while ADHD primarily involves symptoms of inattention, hyperactivity, and impulsivity.

















-template.jpg)



















































































