DMDD Treatment Plan
Create an effective treatment plan for patients with disruptive mood dysregulation disorder (DMDD). Get Carepatron's PDF template for free!


What is disruptive mood dysregulation disorder (DMDD)?
Disruptive mood dysregulation disorder (DMDD) is introduced in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) to address a gap in diagnosing children and adolescents who exhibit chronic severe irritability and frequent intense temper outbursts. This mental health condition goes beyond temporary mood issues; it represents a significant, consistent disruption in the emotional and behavioral state of young individuals. DMDD's core characteristics include a persistently irritable or angry mood interspersed with episodes significantly out of proportion to the situation (American Psychiatric Association, 2013).
Children diagnosed with DMDD often struggle with handling daily stressors and may appear perpetually agitated. These behaviors result in substantial impairments in family, social, and academic environments. It is crucial for mental health professionals to distinguish DMDD from other mental disorders, such as major depressive disorder (MDD), oppositional defiant disorder (ODD), and attention deficit hyperactivity disorder (ADHD), which can also present with irritability and mood dysregulation.
Signs and symptoms of DMDD
Signs and symptoms of DMDD in children and adolescents are marked primarily by severe irritability and frequent, intense temper outbursts (Carlson & Pataki, 2016). These outbursts can manifest both verbally and behaviorally, occurring three or more times a week. DMDD symptoms typically begin before the age of ten and persist across multiple settings, causing significant impairment at home, in school, or during social interactions. This chronic state of irritability is present most of the day, nearly every day, and must be consistent for at least 12 months to warrant a diagnosis.
As youth with DMDD mature, the expression of symptoms may shift; for example, the frequency of temper outbursts might decrease, but DMDD symptoms of anxiety disorders or depressive states may emerge (Benarous et. al., 2020).
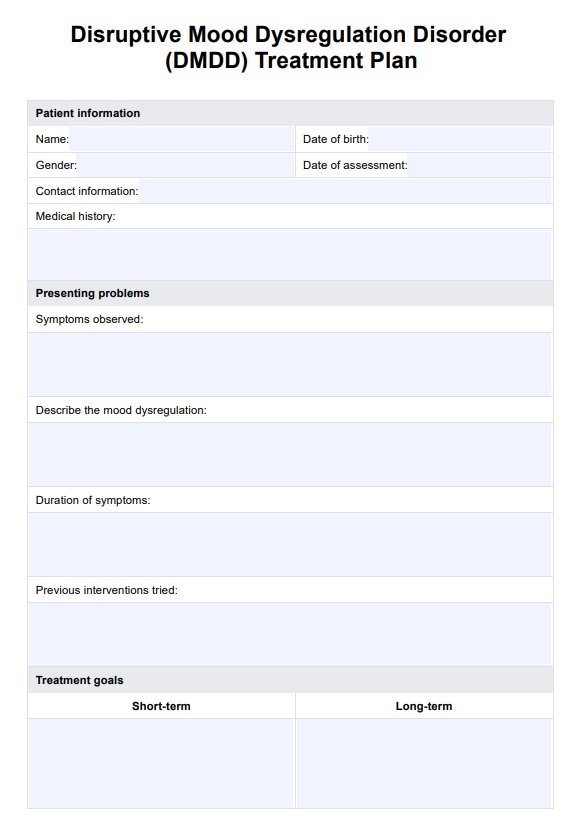
DMDD Treatment Plan Template
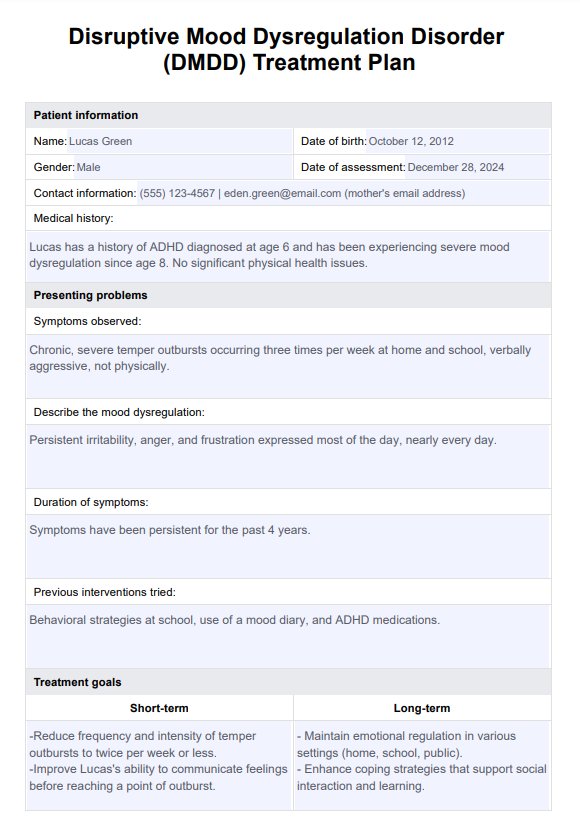
DMDD Treatment Plan Example
How does it work?
Carepatron's free Disruptive Mood Dysregulation Disorder Treatment Plan template is designed for ease and efficiency for professionals to use. Here’s how to use it effectively:
Step 1: Access the template
From this guide, you can choose to "Use template" and access it through the Carepatron platform. You can also select "Download" to get a fillable PDF copy of this treatment plan.
Step 2: Introduce the treatment plan
During your consultation, introduce the DMDD treatment plan, explaining its sections and how each pertains to managing the disorder. This framework helps align treatment expectations.
Step 3: Discuss the treatment plan with the patient and tailor it to their needs
Customize the plan during your discussion, tailoring the treatment strategy to the patient's specific symptoms and life circumstances. This collaborative approach ensures the plan is patient-centered and actionable.
Step 4: Provide further patient education and next steps
Explain the details of the treatment plan, including the interventions like parent training and expected progression. Educate the patient on their role in the treatment process and outline any next steps, such as scheduling follow-up visits or additional assessments. Ensure they fully understand and consent to the proposed treatment.
DMDD treatment
Treatment options for DMDD are developing. Current strategies for managing DMDD borrow extensively from approaches effective in other childhood disorders marked by irritability, such as ADHD, oppositional defiant disorder, and anxiety disorders. The cornerstone of DMDD treatment typically involves psychotherapy, often called talk therapy, which can help children and adolescents develop better stress management techniques and communication skills (National Institute of Mental Health, 2023). In some cases, particularly when symptoms are severe or persist despite psychotherapy, medications may be prescribed to help manage mood swings and irritability.
Recognizing and treating DMDD early with behavioral interventions like parent management training teaches parents to foster positive behavior and decrease irritability. In some cases, atypical antipsychotic medications are used to treat children with irritability associated with DMDD, especially when it co-occurs with other childhood disorders such as autism spectrum disorder or pediatric bipolar disorder.
Given the complexity of DMDD, a combination of psychotherapy and medication might be recommended right from the start. For optimal outcomes, parents and caregivers are advised to collaborate closely with healthcare providers to tailor treatment plans that best meet their child's specific needs.
Benefits of using this treatment plan template
Using the Disruptive Mood Dysregulation Disorder Treatment Plan template offers significant benefits for medical professionals managing patients with this complex mood disorder. This structured approach aids in systematically addressing the varied symptoms and risk factors associated with DMDD, such as chronic irritability, severe outbursts, and depressed mood. By facilitating a comprehensive overview, the plan ensures that all relevant aspects of the disorder, including co-occurring conditions like oppositional defiant disorder (ODD) and potential complications, are considered.
Incorporating evidence-based interventions such as cognitive behavioral therapy (CBT) often referred to as talk therapy, and dialectical behavior therapy (DBT), the template helps you structure your therapeutic approach effectively. These therapies are crucial for helping patients manage irritable behavior and temper tantrums, which can significantly impact life and school performance.
Overall, this treatment plan template optimizes treatment strategies, leading to better management of symptoms and improved patient outcomes. Streamlining the documentation and follow-up process allows you to focus more on care delivery and less on administrative tasks.
References
American Psychiatric Association. (2013). Disruptive mood dysregulation disorder finding a home in DSM. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM-5-Disruptive-Mood-Disregulation-Disorder.pdf
Benarous, X., Renaud, J., Breton, J. J., Cohen, D., Labelle, R., & Guilé, J.-M. (2020). Are youths with disruptive mood dysregulation disorder different from youths with major depressive disorder or persistent depressive disorder? Journal of Affective Disorders, 265, 207–215. https://doi.org/10.1016/j.jad.2020.01.020
Carlson, G. A., & Pataki, C. (2016). Disruptive mood dysregulation disorder among children and adolescents. FOCUS, 14(1), 20–25. https://doi.org/10.1176/appi.focus.20150039
National Institute of Mental Health. (2023). Disruptive mood dysregulation disorder: The basics. https://www.nimh.nih.gov/health/publications/disruptive-mood-dysregulation-disorder
Commonly asked questions
The most effective treatment for DMDD often involves a combination of cognitive behavioral therapy and, if necessary, stimulant medications. Tailored to individual needs, these approaches aim to reduce symptoms, improve emotional regulation, and enhance overall functioning.
No, DMDD is not the same as bipolar disorder; they are distinct conditions. DMDD is characterized by chronic irritability and frequent, severe temper outbursts, while bipolar disorder involves episodic mood changes that include emotional highs (mania) and lows (depression).
While trauma is not specifically identified as a cause of DMDD, stressful life events, and environmental factors can exacerbate or trigger the onset of symptoms in vulnerable children and adolescents.
Triggers for DMDD can include stress at home or school, disruptions in routines, and perceived criticism or failure. Identifying and managing these triggers is a critical component of treatment to help reduce episodes of severe irritability and temper outbursts.

.jpg)
















-template.jpg)






















































































