Mental Health Assessment
Discover how to use a mental health assessment with our guide. Includes a sample template, interpretation, FAQs, and benefits of using a free assessment.


What is a Mental Health Assessment?
A Mental Health Assessment is a comprehensive tool for assessing a person's emotional and psychological well-being. It aids in identifying any mental health issues or conditions that a person may be experiencing. This assessment is not just a snapshot but a detailed picture of a person's mental health. It is also an essential component of mental health treatment because it establishes a baseline for understanding a person's mental health condition.
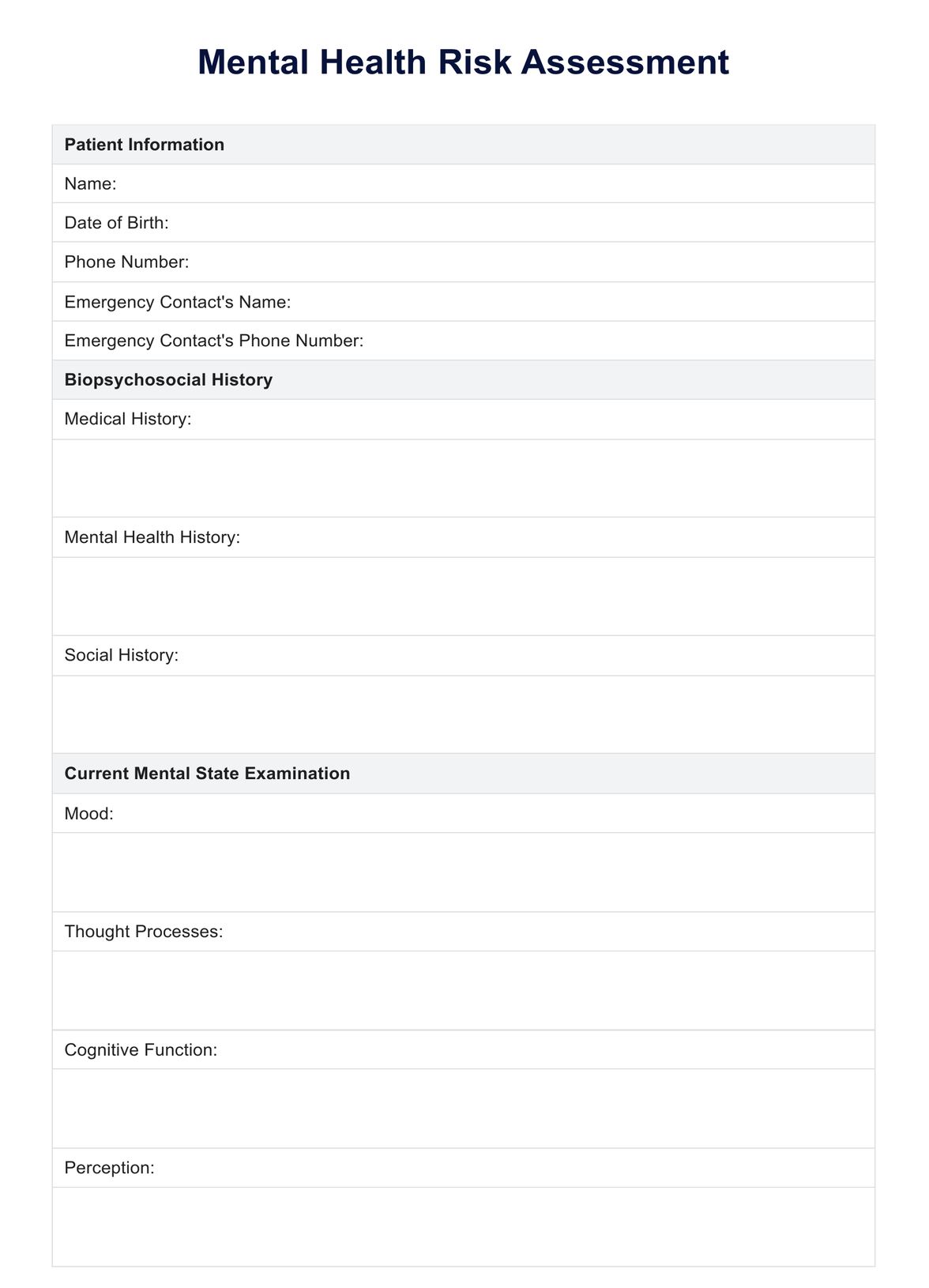
A Mental Health Assessment form uses various methods, including self-assessment questionnaires, clinical interviews, and psychological tests. These evaluation forms assist clinicians and other mental health professionals in understanding the nature and severity of an individual's symptoms and mental health history. They can also be useful in identifying risk and protective factors and determining the best treatment approach.
This assessment can be considered part of the mental health intake process. A mental health specialist can also use it to track treatment progress and determine if any changes are required.
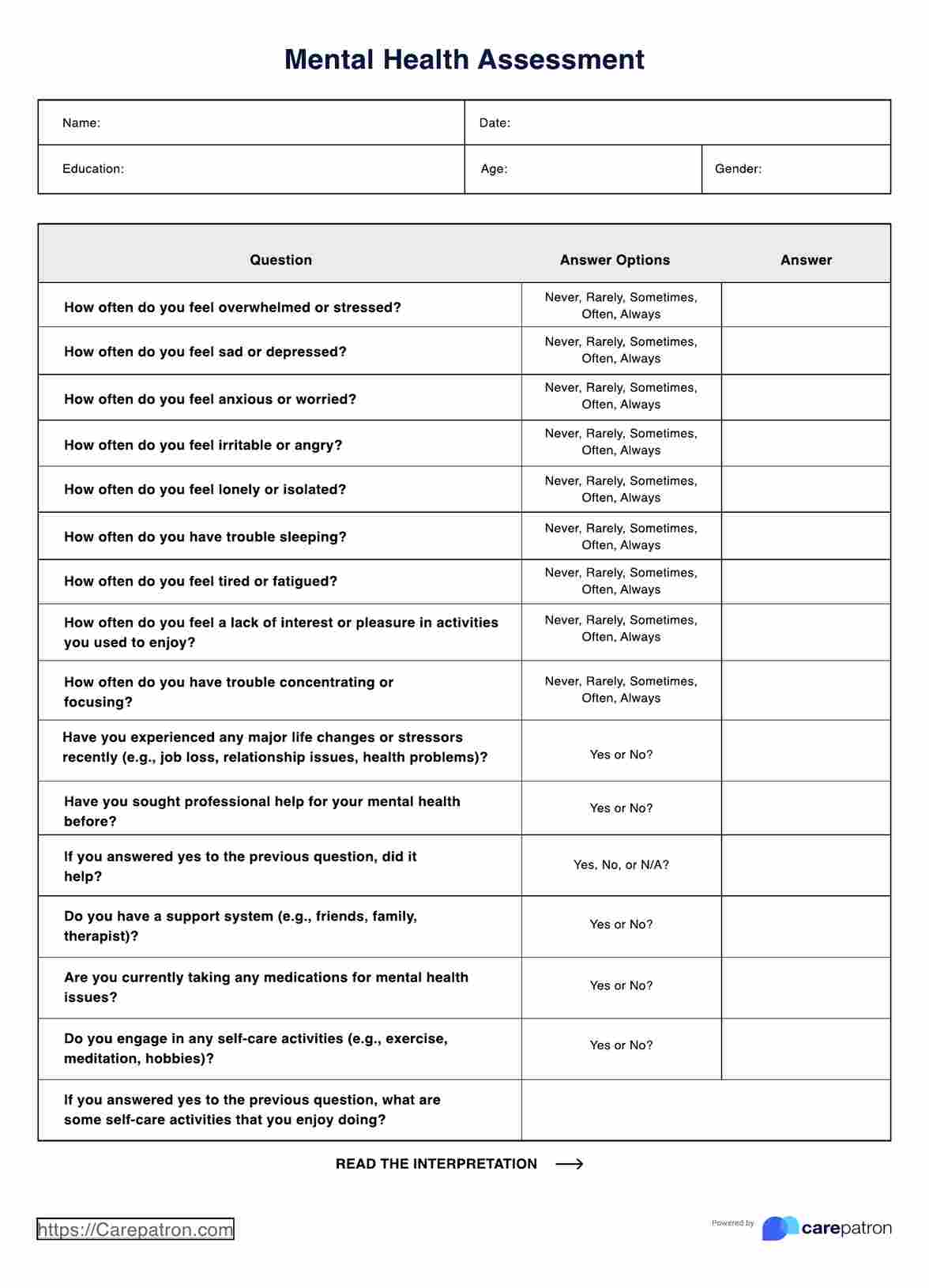
Mental Health Assessment Template
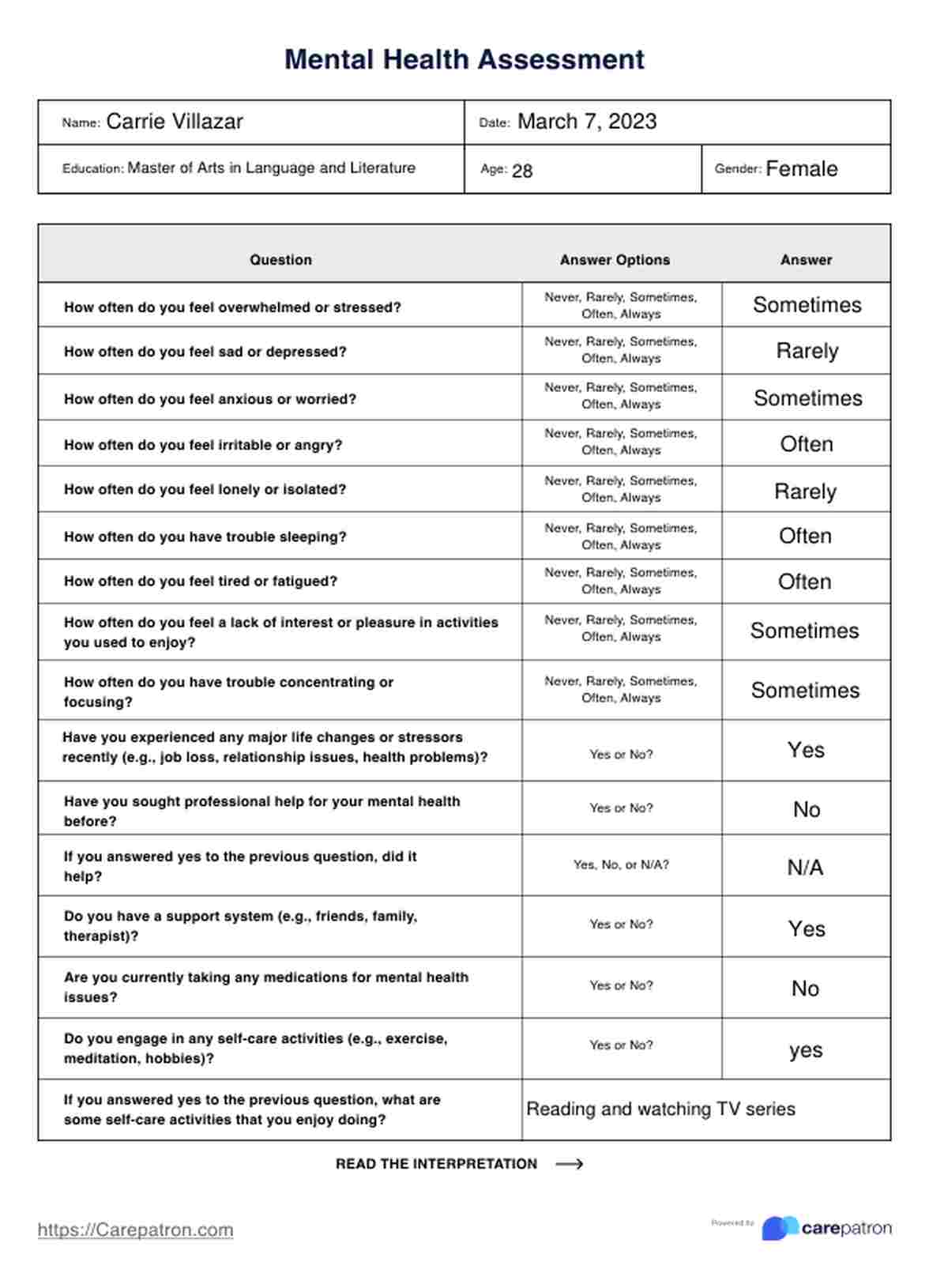
Mental Health Assessment Example
What are common standardized Mental Health Assessment tools?
Mental Health Assessment tools play a crucial role in identifying, diagnosing, and monitoring various mental health conditions and a possible related physical illness. These psychological assessment tools include the following:
- Geriatric Depression Scale: Specifically designed for older adults, the Geriatric Depression Scale (GDS) is a short questionnaire that aims to identify depression in the elderly population. It considers the unique presentation of depressive symptoms in this age group.
- Patient Health Questionnaire-9(PHQ-9): A brief, self-administered tool that assesses the severity of depression based on the DSM-IV criteria. Patient Health Questionnaire-9(PHQ-9) is widely used in primary care settings and can help track treatment progress.
- Beck Depression Inventory (BDI): Beck Depression Inventory is a 21-item self-report questionnaire assesses the severity of depression symptoms in adolescents and adults. It covers key aspects such as mood, pessimism, and loss of pleasure.
- SCOFF Questionnaire: SCOFF Questionnaire is simple, five-question screening test for eating disorders that can be easily administered in primary care settings.
- Dissociative Experiences Scale(DES): Dissociative Experiences Scale (DES) consists of 28 items covering various dissociative symptoms, such as depersonalization and derealization.
- Life events checklist (LEC): This self-report measure includes 17 items covering various traumatic experiences, such as natural disasters, accidents, and interpersonal violence.
- Mood Disorder Questionnaire(MDQ): Mood Disorder Questionnaire is a brief, self-report screening instrument for bipolar spectrum disorders. It assesses symptoms of mania or hypomania.
- Panic Disorder Severity Scale(PDSS): The Panic Disorder Severity Scale (PDSS) evaluates various aspects of panic attacks, including frequency, distress, and impact on daily functioning.
When used in conjunction with in-depth clinical interviews tackling family history, medical history, and drug and alcohol use, as well as previous experience with a mental health problem, these psychological testing tools contribute to a comprehensive understanding of a patient's status to improve their overall mental well-being.
How to use this Mental Health Assessment
This Mental Health Assessment template can be useful in clinical and psychiatric practice. Here's a step-by-step guide to using and filling out this assessment:
Step 1: Download and print the free template
The free template is downloaded and printed as the first step in using the Mental Health Assessment. It is easily accessible online and available in PDF format.
Step 2: Explain how it works
Give your client a copy and explain how the assessment works. Inform them that it consists of questions about their current well-being, lifestyle, physical health, and other factors, which will help identify potential issues.
Step 3: Encourage honesty
As a mental health provider, you should encourage your client to be honest and open while completing the assessment. Assure their answers are confidential and will only be used for treatment.
Step 4: Review the results together
After your client completes this patient health questionnaire, review the answers together. This is an opportunity to discuss any concerns or patterns that may have emerged from the assessment and determine if further evaluation or treatment is needed.
When is a Mental Health Assessment needed?
A Mental Health Assessment becomes essential in various circumstances, serving as a valuable tool to identify, understand, and address mental health concerns.
Symptoms of mental health conditions
If an individual is experiencing symptoms of mental health conditions such as depression, anxiety, post-traumatic stress disorder (PTSD), mood disorders, attention-deficit/hyperactivity disorder (ADHD), generalized anxiety disorder, or other mental health disorders, a Mental Health Assessment is warranted. This can help provide a general baseline that can be used with lab tests for accurate diagnosis and treatment planning.
Onset of mental health disorders
In cases where there is a suspected onset of mental disorders or cognitive impairment, seeking the expertise of a mental illness professional becomes imperative. Early assessment can aid in prompt diagnosis and developing an effective treatment plan.
Prior history of mental illness
Individuals with a prior history of mental illness or with family members who have one can undergo regular Mental Health Assessments to monitor their well-being and identify any emerging challenges. This proactive approach can contribute to long-term mental health management.
Seeking professional guidance
When individuals feel overwhelmed, stressed, or find it challenging to cope with life's demands, they should consult a mental health provider for an assessment. This step can help address underlying issues and provide coping strategies.
Requirement for mental health tests
Employers, educational institutions, or legal entities may require individuals to undergo these screening measures or tests in certain situations. Compliance with these requests is crucial for continued well-being and meeting specific criteria.
Commonly asked questions
A comprehensive Mental Health Assessment gathers information about the client's presenting problems, mental health history, medical history, family history, substance use, safety concerns, and treatment goals. It may involve standardized screening tools, a mental status exam, and a diagnostic interview.
When documenting a Mental Health Assessment, you can use a structured SOAP note format that includes the Subjective section to record the client's self-reported symptoms, concerns, and goals in their own words; the Objective section to document observable signs and behaviors during the assessment; the Assessment section to provide your clinical impressions; and the Plan section to outline the recommended treatment approach.
The time required to complete a Mental Health Assessment can vary depending on the setting and the client's specific needs. A thorough initial assessment may take 30-60 minutes or longer. Follow-up assessments are typically shorter and focus on monitoring progress and adjusting the treatment plan.
















-template.jpg)






















































































