Prepatellar Bursitis Treatment Guidelines Handout
Our handout for guidelines on treating prepatellar bursitis helps promote recovery. Use our template today, great for quick reference and patient education.


What is prepatellar bursitis?
Prepatellar bursitis is an inflammation of a small fluid-filled sac known as the prepatellar bursa, named so because it is in front of the patellar tendon. This sac of soft tissues acts as a cushion to help reduce friction. Activity such as repetitive kneeling, multiple knee injuries, or acute trauma causes the bursa to become irritated and fill with fluid, resulting in knee pain and swelling.
There are two main types of prepatellar bursitis:
- Aseptic prepatellar bursitis: non-infectious
- Septic prepatellar bursitis: also called infectious bursitis, this often involves bacteria like Staphylococcus aureus and likely requires immediate treatment.
Those at most risk of developing prepatellar bursitis include individuals whose work involves frequent kneeling like gardeners and roofers, which is why it's called housemaid's knee (or similar variants, such as carpet-layers' knee or carpenter's knee). Other individuals at higher risk include athletes, patients with underlying conditions such as rheumatoid arthritis and gout, and immunosuppressed patients. This includes patients with diabetes mellitus, those who engage in chronic steroid use, and those undergoing hemodialysis.
Symptoms of an inflamed bursa can include localized swelling, tenderness, and restricted range of motion of knee movements. In cases of prepatellar septic bursitis, patients may experience erythema, warmth, and fever due to the presence of infection.
Diagnosis of prepatellar bursitis typically starts with a physical examination to assess localized swelling, pain, and the affected knee’s range of motion. Clinicians may palpate the area for tenderness and use imaging (e.g., X-rays or MRI) to rule out fractures or other conditions. In cases where infection is suspected, fluid aspiration and lab analysis help diagnose prepatellar bursitis, distinguishing septic from aseptic cases.
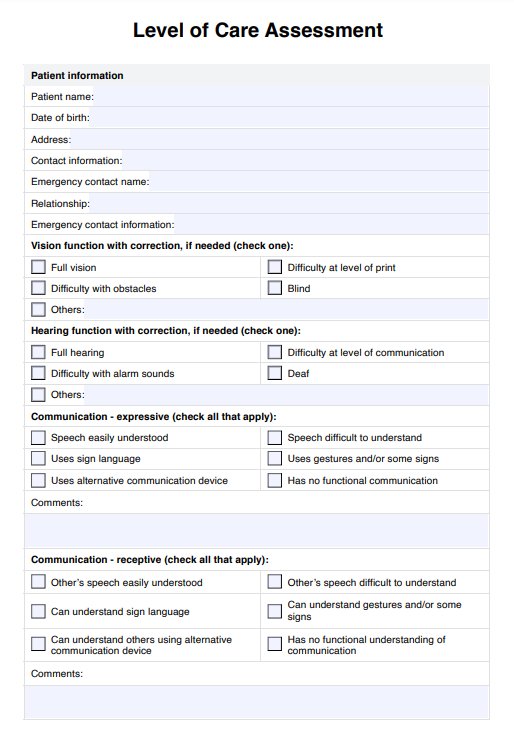
Prepatellar Bursitis Treatment Guidelines Handout Template
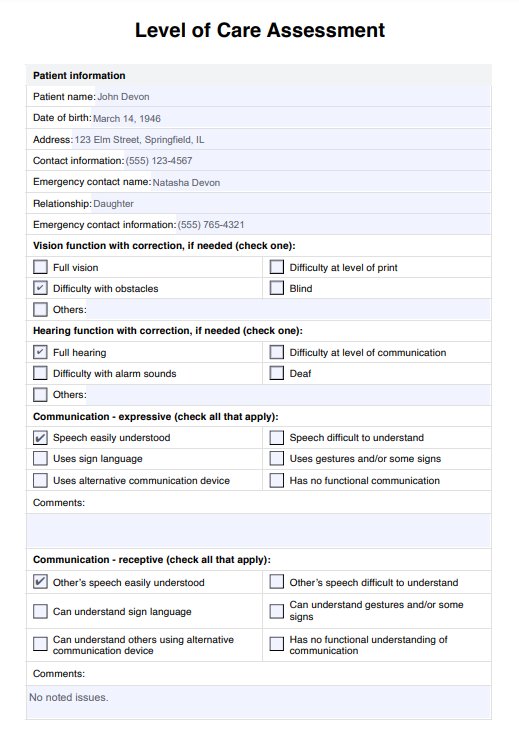
Prepatellar Bursitis Treatment Guidelines Handout Example
How to use our treatment guidelines handout template?
Our Prepatellar Bursitis Treatment Guidelines Handout provides a comprehensive outline of treatment approaches for prepatellar bursitis, along with a sagittal knee diagram for easy bursa location. Use the following steps to integrate this handout into your care:
Step 1: Access the template
Click “Use template” to open the handout within the Carepatron app, allowing you to customize, share, and securely store the document. Alternatively, use “Download” for a printable PDF.
Step 2: Assess the patient
Conduct a thorough assessment of the patient's affected knee. Use the sagittal diagram to locate the bursa and communicate the condition’s impact to the patient.
Step 3: Discuss treatment options
Review the home and professional treatments listed on the handout. Outline specific interventions for the patient, such as rest, activity modification, or medical options for more severe cases.
Step 4: Educate the patient for self-management
Explain each treatment step, including home remedies and when professional care is necessary. Encourage the patient to use the handout for self-care tracking and to contact their provider with any worsening symptoms.
Treatment for prepatellar bursitis
Effective management of prepatellar bursitis involves both home remedies and professional treatments, depending on the severity of the condition. Addressing symptoms such as knee swelling and pain, these options range from non-surgical treatments to endoscopic excision for severe cases.
Rest and activity modification
Resting the affected knee and avoiding aggravating activities, like kneeling or squatting, are essential first steps. Adjusting daily activities can help relieve pain and prevent prepatellar bursitis from worsening, allowing the inflammation to subside. You may also use or wear protective equipment like knee pads or mats.
Ice therapy
Applying an ice pack for 15–20 minutes every few hours helps reduce knee swelling and other symptoms of acute prepatellar bursitis. Ensure the ice pack is wrapped in a cloth to avoid frostbite on the skin.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Over-the-counter NSAIDs, such as ibuprofen, relieve pain and inflammation in mild cases. These anti-inflammatory drugs support treating acute prepatellar bursitis symptoms and aid in pain management, although they are generally a temporary measure rather than a long-term solution.
Aspiration
In cases of significant swelling, a healthcare provider may drain excess fluid from the bursa through aspiration. This non-surgical treatment can relieve pain and pressure, providing insight into any possible infection in the bursa.
Corticosteroid injections
For persistent inflammation that does not respond to home care, a corticosteroid injection (such as a triamcinolone or cortisone injection) may be administered to reduce knee swelling and inflammation. These injections may relieve pain in severe cases of prepatellar bursitis but are avoided during pregnancy and for those with diabetes.
Incision and drainage
When infection leads to abscess formation, a minor surgical procedure to drain the bursa may be required. Incision and drainage relieve pressure, treat infection, and promote healing.
Antibiotic therapy
If septic prepatellar bursitis is present, intravenous antibiotics may be prescribed, such as vancomycin or ceftriaxone. These antibiotics target infection directly, and their dosage may need adjustments for patients with kidney issues.
Sclerotherapy and bursectomy
For chronic or recurrent bursitis, sclerotherapy or bursectomy may be advised. Sclerotherapy involves injecting a chemical agent to shrink the bursa, while bursectomy involves surgically removing it to prevent recurrence. Both treatments are generally avoided for pregnant patients.
Endoscopic excision
Endoscopic treatment of prepatellar bursitis is a minimally invasive approach to surgically removing the bursa with minimal downtime. This method is effective in chronic cases, providing a long-term solution by reducing recurrent inflammation in the knee.
After recovery, patients are advised to engage in physical therapy to strengthen surrounding muscles and improve knee stability. Building strength in the leg muscles, particularly the quadriceps, helps prevent prepatellar bursitis recurrence by enhancing joint stability and reducing strain on the affected knee.
Benefits of using this handout
Our Prepatellar Bursitis Handout provides essential information for effective treatment and patient education, helping both healthcare professionals and patients manage this condition with clarity.
- Clear treatment steps: Provides straightforward instructions for both home remedies and professional treatment options, ensuring easy application in patient care.
- Informs on symptoms and risks: Guides patients in identifying symptoms and understanding risk factors, which promotes proactive management.
- Supports personalized care: Allows healthcare providers to tailor treatments based on individual patient needs and preferences.
- Easy access and use: Available in printable and digital formats for convenient reference in clinical or home settings.
Commonly asked questions
In many cases, prepatellar bursitis can resolve on its own, especially with rest and home treatments such as ice and activity modification. However, if the bursitis is due to infection and not because of a knee injury, or if symptoms persist despite self-care, treatment by a healthcare professional may be necessary to avoid complications and promote recovery.
The first line of treatment for bursitis typically involves conservative measures, such as rest, ice application, and over-the-counter anti-inflammatory medications to manage pain and reduce swelling. These approaches are effective for most kinds of soft tissue injury, allowing inflammation to subside and healing to begin.
The best treatment for prepatellar bursitis depends on the severity of the condition. Mild cases usually respond well to rest, ice, and non-steroidal anti-inflammation drugs (NSAIDs), while more severe or persistent cases may require aspiration, corticosteroid injections, or even surgery. The appropriate knee bursitis treatment should be guided by the underlying cause and the patient’s response to initial therapies.