The first line of treatment for schizophrenia typically includes antipsychotic medications, which can help manage symptoms such as delusions and hallucinations. Psychosocial treatments, such as therapy, support groups, and vocational training, are also often recommended to address social and behavioral issues.
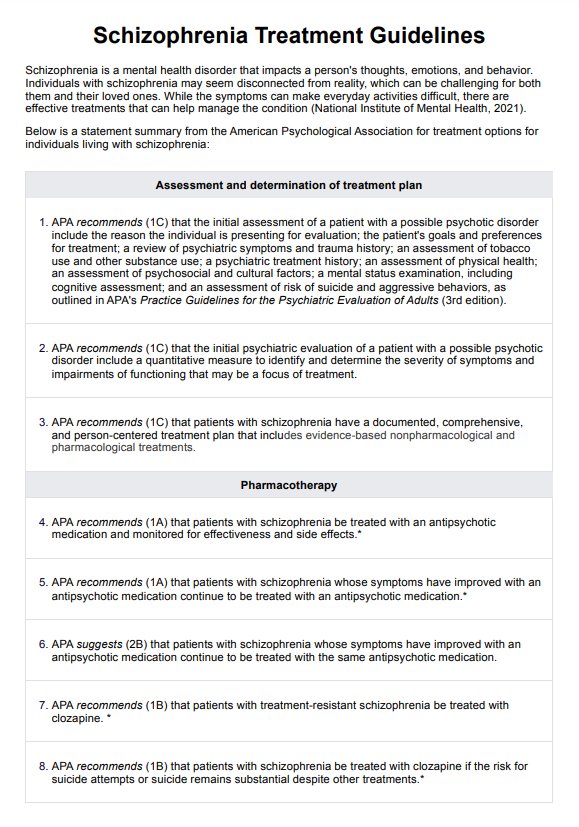
Schizophrenia Treatment Guidelines
Stay informed with the latest Schizophrenia Treatment Guidelines for comprehensive care and a deeper understanding of available treatment options.
Schizophrenia Treatment Guidelines Template
Commonly asked questions
Schizoaffective disorder and schizophrenia are both severe mental health conditions but differ mainly in their symptom profile. Schizophrenia is characterized primarily by psychotic symptoms and mental disorders such as delusions, hallucinations, and disorganized thinking.
The best treatment protocol for schizophrenia typically involves a combination of antipsychotic medication and psychosocial treatments. Medication helps to manage the acute symptoms and prevent relapses. Cognitive therapy, behavioral therapy, social skills training, and supported employment can help with social functioning and quality of life.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











